An interview with Dr Christiana Demetriou, Assistant Professor of Epidemiology and Public Health and MPH Programme Coordinator.
by Constandinos Tsindas
How do you see the pandemic situation? Are we moving in the right direction and how concerned are you?
Definitely an exciting and challenging time. Throughout the past year, we’ve seen how epidemiology has shaped the COVID-19 pandemic; from sounding the alarm following reports of a previously unknown coronavirus causing pneumonia-like symptoms, to modelling the transmissibility of the virus and the impact of control measures, to testing and rolling out several vaccines specific to the new virus, to now predicting the impact of new variants of the virus.
In fact, thinking of what the scientific community has achieved in this past year, while navigating unprecedented circumstances, cannot but leave one in awe! Therefore, we are definitely doing many things right and we are moving in the right direction.
While discussing with other scientists, I think the consensus is that we have quite a long road ahead of us. The main concerns right now are how to achieve sufficient vaccine coverage, as high a percentage of people vaccinated as possible. And of course, while working towards understanding how effective existing vaccines are against new viral strains. We’ve won many a battle, but the war is far from over.
What are your views and proposals on how to move forward?
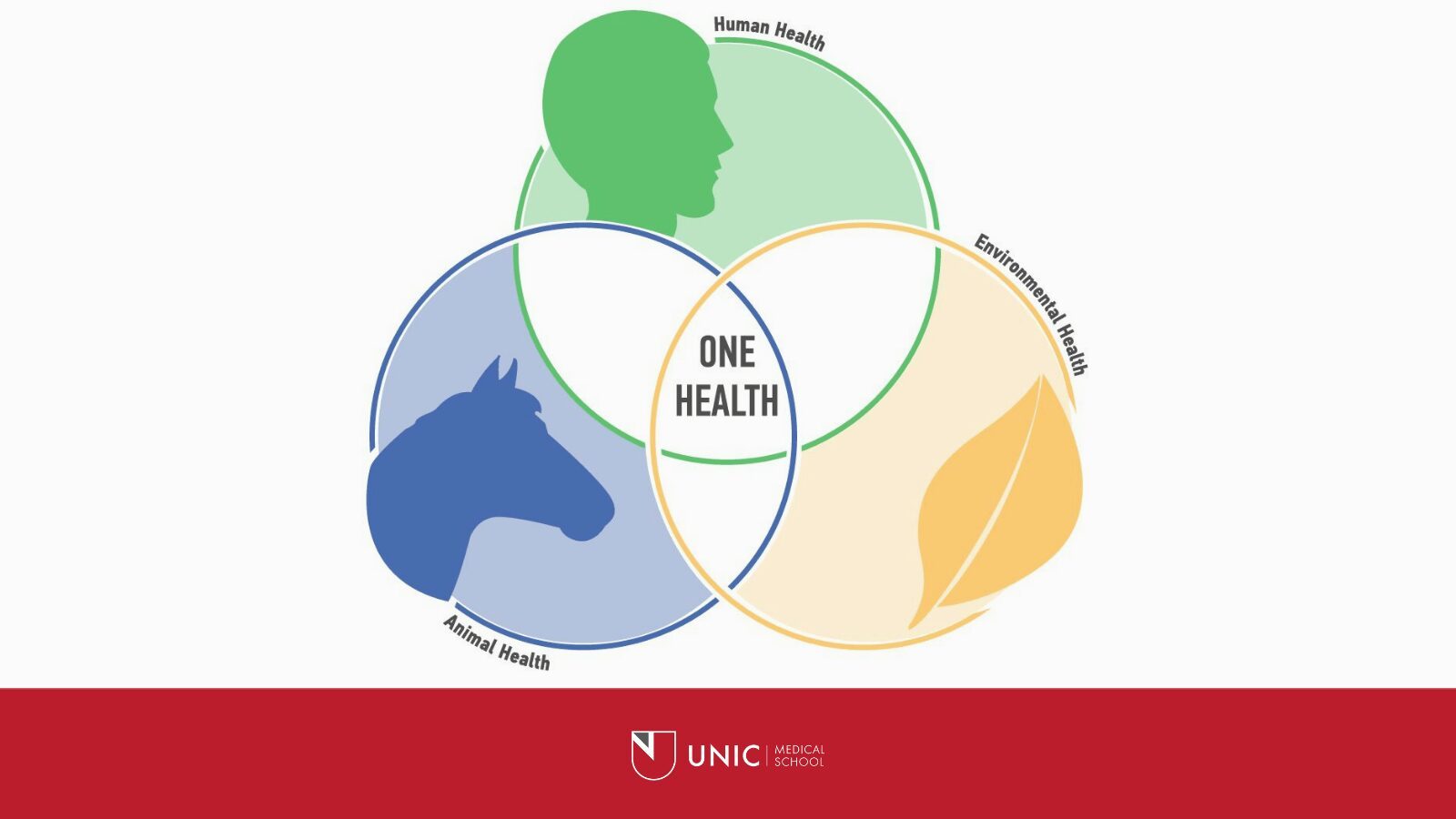
Public Health needs to more actively acknowledge and embrace the interconnectedness between human health, animal health and environmental health. You cannot have the one without the other and that’s why this is often referred to as the One Health concept. For years, humans have strived for their wellbeing often disregarding the impact on nature and the environment. This has led to climate change, geologic, hydrologic and meteorological disasters, anti-microbial resistance and, currently, epidemics of emerging zoonotic diseases.
If we really want to improve, we need to consider the holistic approach of the One Health concept.
Importantly, Public Health needs to pay more attention to health inequalities both between but also within countries. Even in countries with the highest sociodemographic indices, there exist astounding health inequalities between population groups. As a mother, what pains me the most is that children are often born in inequality; with the genetic, lifestyle and socio-economic conditions of their parents determining their maximum potential in terms of health attainment.
In future, I would like to see Public Health addressing these health inequalities by focusing more on the wider determinants of health and their impact on the conditions of future generations.
Do you believe we need to bring the whole public health system down in terms of its approach and build a new one? Or work through this one?
I am more in favour of reforming, rather than demolishing and rebuilding! The discipline of Public Health has made tremendous progress in the past few decades. We only need to look at the differences in life expectancies, what 30 to 40 years ago and today to clearly witness the advancements made.
Interestingly, most of science happens under controlled conditions, for example in a laboratory, in a petri-dish, in a randomized controlled clinical trial. Unfortunately, when it comes to improving population health, the human factor makes the conditions we have to work with, anything but controlled; anything but ideal! Therefore, we need to learn from the achievements and even some failures of the past to continue tackling the pertinent issues in Public Health.
This is actually one of the reasons why I am so proud of my job. We, the MPH programme that is, get to contribute to this reformation and advancement, through the training of the future generation of public health professionals.
What are you currently working on in terms of epidemiological research and clinical trials?
Not surprisingly, most of my current research activity is “consumed” with COVID-19. I am the Principal Investigator of the C-MOR project, coordinated by the University of Nicosia Medical School.
It consists of an international consortium of partners who came together with the aim of creating a reference dataset focused on mortality resulting from COVID-19 (https://www.unic.ac.cy/coronavirus/mortality/).
Currently, the project has more than 50 partners from countries across six continents. Some of our objectives are to investigate excess all-cause mortality during the COVID-19 pandemic, identify the percentage contribution of COVID-19 deaths to the excess mortality, disentangle direct and indirect excess mortality due to COVID-19, and investigate excess mortality in the context of country specific COVID-19 control measures. Our initial results – based on data from March until August 2020 – highlight the importance of mortality surveillance in studying the burden of COVID-19, as well as the impact of COVID-19 control measures on the mortality experience of different countries. These results have been accepted for publication in the “International Journal of Epidemiology” which is a peer reviewed academic journal with high impact and high visibility in the field of Epidemiology, Public Health and Medicine. In addition, using mortality data from contributing partners we managed to show that COVID-19 contributed to premature mortality in almost all countries investigated, but to varying degrees. Currently, data spanning the whole of 2020 is being gathered so as to be able to get a more representative picture of the impact of COVID-19 and also to study different waves of the pandemic in the participating countries.
Perhaps closer to my research background, chronic disease epidemiology, I am currently also involved in a project investigating the epidemiology of cancer in Cyprus. We are looking into temporal trends as well as any inequalities in the stages at which different cancers are diagnosed in different population groups. We also hope that the project will highlight the effectiveness of established and newly implemented cancer screening programmes. This project is in collaboration with the Ministry of Health Cancer Registry.
As a scientist, what do you think about the future?
Definitely optimistic and hopeful! I take pride in the advancements achieved by the discipline of Public health, and the scientific community, to date. I am hopeful that the lessons learned will enable us to continue to tackle the often-wicked problems of Public Health. Perhaps most importantly, I cannot but be optimistic when I see all our students who have dedicated their studies and professional lives to improving population health! With this kind of woman- and man-power, and ultimately, Human Power, I am certain that we’re in for a bright Public Health future.
As Owen Arthur said, “For he who has health has hope; and he who has hope, has everything.”